Anesthesia and Myocardial Ryanodine Receptors
May 16, 2022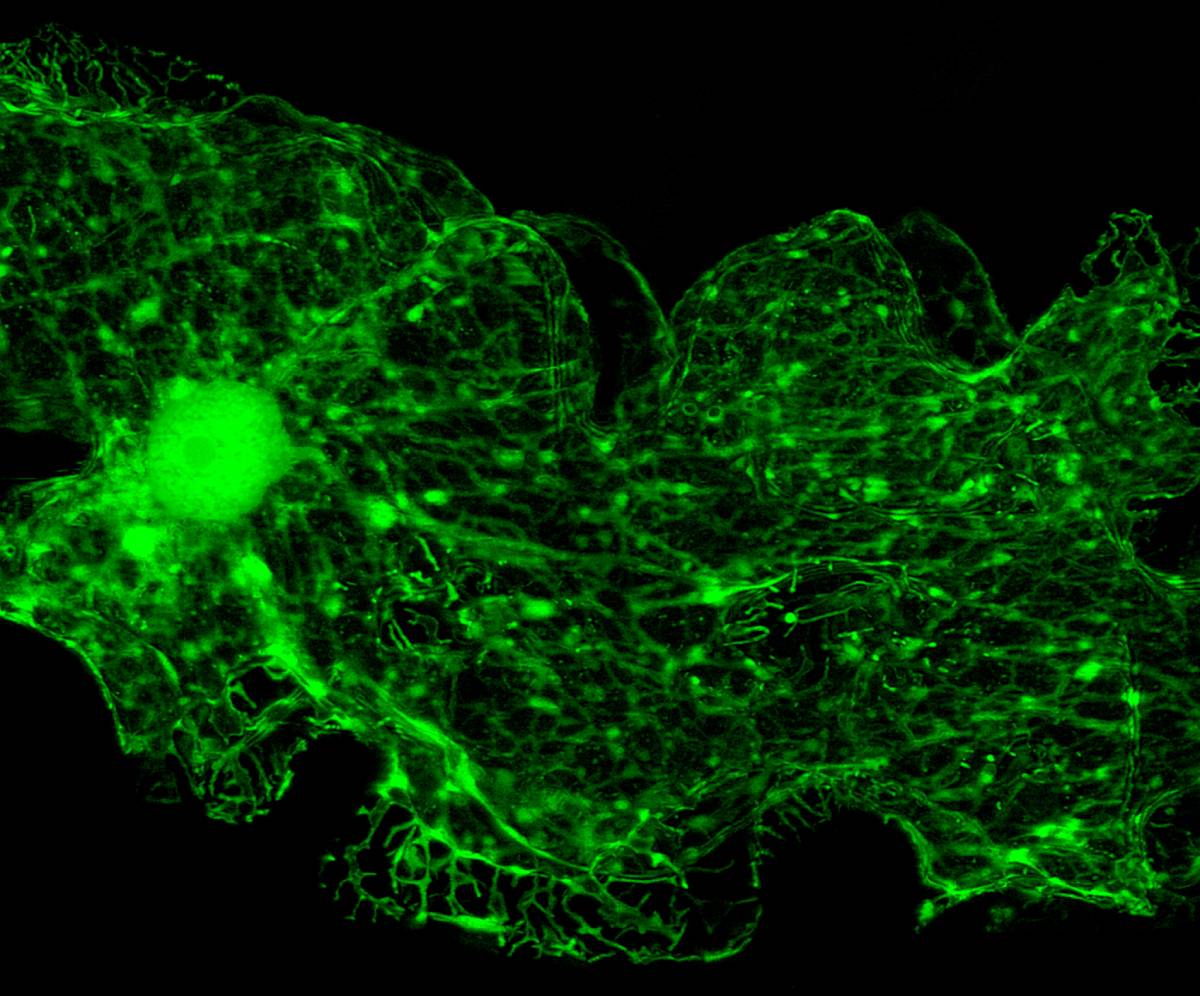
Cardiovascular complications are the primary cause of morbidity in developed countries; Anesthetics can have cardiovascular effects, making the choice of anesthesia in the operating room particularly important. Volatile anesthetics such as sevoflurane and isoflurane have caused myocardial depression and led to hemodynamic instability at higher doses [1]. These volatile anesthetics have also been shown to be cardioprotective during ischemia/reperfusion injury. Similar to other forms of cardioprotection, desflurane or isoflurane can prevent mitochondrial Ca2+-induced Ca2+ release in cardiac tissue through mitochondrial translocation of protein kinase C epsilon (PKCε) [2]. On the other hand, general anesthesia can also cause abnormal cardiac repolarization, as identified by prolonged QT intervals on an electrocardiogram. Drug-induced QT prolongation increases the risk of malignant tachyarrhythmias such as torsades de pointes and sudden cardiac death [3]. Myocardial ryanodine receptors have been identified as a key component in the effect of anesthesia on the heart.
Ryanodine receptor 2 (RyR2) are Ca2+ release channels in the myocardium, the inner, muscular part of the heart. They are responsible for Ca2+-induced Ca2+ release in cardiac muscle cells. Once released from the sarcoplasmic reticulum, calcium activates the myofilaments and initiates contractions [4]. A slow Ca2+ release could inhibit myocardial relaxation and induce diastolic dysfunction. Additionally, persistent RyR2 opening may be arrhythmogenic and increases the risk of ventricular fibrillation [5].
An Australian preclinical study isolated ryanodine receptors from healthy sheep hearts and transferred them to artificial lipid bilayers, after which their gating properties were measured in response to volatile anesthesia [6]. Most half-maximal activating concentrations (Ka) had constant low values around 1.5 mM, except for isoflurane, which had a Ka of 5.3 mM. Under these conditions, RyR2 opening activity increased by 120% with halothane administration, 50% with enflurane and desflurane, and insignificantly with isoflurane and sevoflurane [6]. If administered along with isoflurane, sevoflurane, desflurane, or enflurane, the muscle relaxer dantrolene negates any RyR2 activating effect entirely. With their results in mind, the authors suggest isoflurane-based anesthesia would be best in patients where increasing ryanodine receptor activity and reducing cardiac function would be detrimental. In cases where RyR2 activation would be beneficial (for example, in patients with cardiac ischemia, increased RyR2 activity can be cardioprotective), the authors suggest using a sevoflurane or desflurane-based regimen [6].
After exploring the mechanism of action, the authors show the increasing effect of halothane persists independent of ATP, contradicting a previous finding [7]. The largest effect of halothane was its potentiation of luminal Ca2+ activation of RyR2 during both systole and diastole. Previous studies suggested that luminal Ca2+ may permeate the open RyR2 pore and bind to cytoplasmic facing sites, thus maintaining channel opening for sustained periods of time [8].
Mice anesthetized with ketamine and subjected to ischemic-reperfusion injury were also administered the free radical scavenger MPG. It was shown that avoiding RyR2 oxidation with MPG reduced the frequency of arrhythmias and did not change cardiac contractility [9]. A clinical study indicated individuals with catecholaminergic polymorphic ventricular tachycardia (CVPT) may benefit from flecainide, a class 1 antiarrhythmic drug with anesthetic action. The researchers provided evidence that the antiarrhythmic action was via inhibition of cardiac RyR2 and subsequent reduction of Ca2+ release during diastole [10].
While interesting, these studies can be expanded on in the future to investigate different anesthetic agents. Besides volatile anesthetics, propofol, dexmedetomidine and opioids are also commonly used during anesthesia and may affect cardiac ryanodine receptors. By highlighting the need for personalized anesthesia regimens, the authors offer a solid platform on which further research can be conducted.
References
- Malan, T. P., DiNardo, J. A., Isner, R. J., Frink, E. J., Goldberg, M., Fenster, P. E., Brown, E. A., Depa, R., Hammond, L. C., & Mata, H. (1995). Cardiovascular Effects of Sevoflurane Compared with Those of Isoflurane in Volunteers. Anesthesiology, 83(5), 918–928. https://doi.org/10.1097/00000542-199511000-00004
- Lotz, C., & Kehl, F. (2015). Volatile Anesthetic-induced Cardiac Protection: Molecular Mechanisms, Clinical Aspects, and Interactions with Nonvolatile Agents. Journal of Cardiothoracic and Vascular Anesthesia, 29(3), 749–760. https://doi.org/10.1053/j.jvca.2014.11.012
- Nagele, P., Pal, S., Brown, F., Blood, J., Miller, J. P., & Johnston, J. (2012). Postoperative QT Interval Prolongation in Patients Undergoing Noncardiac Surgery under General Anesthesia. Anesthesiology, 117(2), 321–328. https://doi.org/10.1097/ALN.0b013e31825e6eb3
- Hobai, I. A. (2017). Anesthetics, the Ryanodine Receptors, and the Heart. Anesthesiology, 126(3), 373–375. https://doi.org/10.1097/ALN.0000000000001520
- Venetucci, L., Denegri, M., Napolitano, C., & Priori, S. G. (2012). Inherited Calcium Channelopathies in the Pathophysiology of Arrhythmias. Nature Reviews Cardiology, 9(10), 561–575. https://doi.org/10.1038/nrcardio.2012.93
- Laver, D. R., Attia, J., Oldmeadow, C., & Quail, A. W. (2017). Cardiac Calcium Release Channel (Ryanodine Receptor 2) Regulation by Halogenated Anesthetics. Anesthesiology, 126(3), 495–506. https://doi.org/10.1097/ALN.0000000000001519
- Yang, Z., Harrison, S., & Steele, D. (2005). ATP-dependent Effects of Halothane on SR Ca2+ Regulation in Permeabilized Atrial Myocytes. Cardiovascular Research, 65(1), 167–176. https://doi.org/10.1016/j.cardiores.2004.09.00
- Györke, I., & Györke, S. (1998). Regulation of the Cardiac Ryanodine Receptor Channel by Luminal Ca2+ Involves Luminal Ca2+ Sensing Sites. Biophysical Journal, 75(6), 2801–2810. https://doi.org/10.1016/S0006-3495(98)77723-9
- Becerra, R., Román, B., Di Carlo, M. N., Mariangelo, J. I., Salas, M., Sanchez, G., Donoso, P., Schinella, G. R., Vittone, L., Wehrens, X. H., Mundiña-Weilenmann, C., & Said, M. (2016). Reversible Redox Modifications of Ryanodine Receptor Ameliorate Ventricular Arrhythmias in the Ischemic-Reperfused Heart. American Journal of Physiology-Heart and Circulatory Physiology, 311(3), H713–H724. https://doi.org/10.1152/ajpheart.00142.2016
- Smith, G. L., & MacQuaide, N. (2015). The Direct Actions of Flecainide on the Human Cardiac Ryanodine Receptor. Circulation Research, 116(8), 1284–1286. https://doi.org/10.1161/CIRCRESAHA.115.306298