Gut Microbiome and Anesthesia
March 20, 2023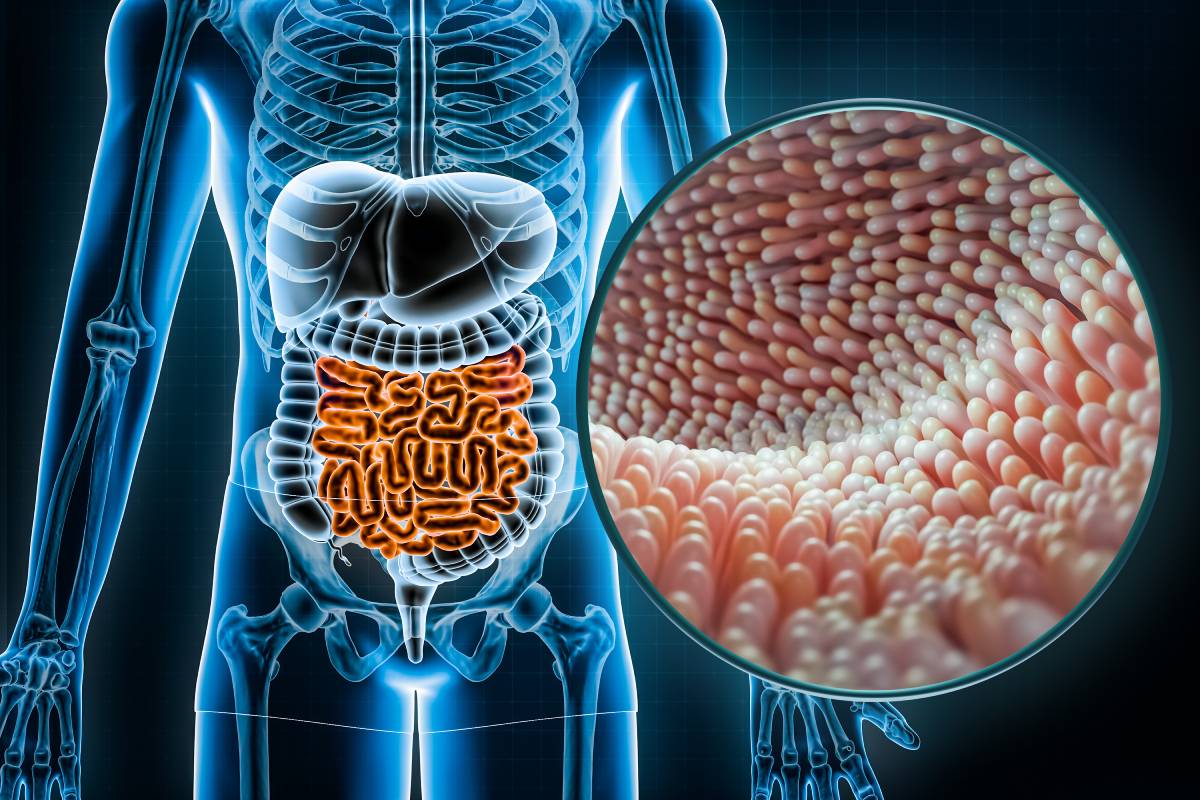
Recent studies suggest that the gut microbiome, which has increasingly been found to be related to aspects of health outside the gastrointestinal system, may play a role in anesthesia and pain medicine. The gut microbiome refers to the complex community of microorganisms that live in the gastrointestinal tract. It is known to interact with the nervous system, which governs pain sensations, via the gut-brain axis.
The gut-brain axis is a bidirectional communication system between the gastrointestinal tract and the central nervous system (CNS) that allows gut microbiota to influence the CNS through several pathways, including the vagus nerve and enteric nervous system, immune system modulation, metabolite production and endocrine signaling. 1,3 Liang Xu et al. explains that the multi-organ interaction of the CNS with the ENS (enteric nervous system) creates the gut-pain axis and leads to paired diseases, for example, anxiety and depression are associated with inflammatory bowel disease.3 In humans, a randomized controlled trial found that a probiotic supplement reduced pain in patients with irritable bowel syndrome (IBS), a chronic condition characterized by abdominal pain and altered bowel habits.1,3
Minerbi and Shen and discuss using fecal microbiota transplantation (FMT) for the treatment of a wide range of gastrointestinal and immune-related disorders. FMT is being investigated because it influences the pathway by which the gut microbiome modulates pain via the immune system. Gut microbiota can create changes in immune cell populations and cytokine production. These changes can ultimately affect the CNS (central nervous system) and lead to altered pain perception. Gut microbiota can also produce metabolites, such as short-chain fatty acids (SCFAs), that can affect pain perception. SCFAs can activate receptors in the gut-brain axis and modulate neuronal activity, ultimately leading to changes in pain sensitivity. In addition to its role in pain management, the gut microbiome has also been implicated in anesthesia since it can affect the pharmacokinetics and pharmacodynamics of anesthetic drugs. The gut microbiota can modulate drug absorption and metabolism, leading to altered drug concentrations and effects. For example, Minerbi and Shen found that alterations in the gut microbiome can affect the metabolism of propofol, a commonly used anesthetic agent. Additionally, the gut microbiome has been shown to influence the immune response to anesthetic agents, potentially affecting the risk of adverse events.1
Weersma et al. is hopeful that the bidirectional nature of this interaction holds many opportunities for enhancing therapeutic drug delivery.2 While proton pump inhibitors (PPI) and antibiotics negatively impact the gut microbiome, disrupting the same lipid biosynthesis pathways in the gut that affect pain perception, many scientists hypothesize that these pathways can be positively manipulated to improve patient health outcomes.2 Overall, the gut microbiome is an emerging area of interest. While there is still much to learn about the complex interactions between the gut microbiome and these medical specialties, early research suggests that the gut microbiome may play a significant role in making healthcare more personalized. Further research is needed to better understand these interactions and to explore the potential for microbiome-based interventions in anesthesia and pain medicine. 1
References
1. Amir Minerbi, Shiqian Shen; Gut Microbiome in Anesthesiology and Pain Medicine. Anesthesiology 2022; 137:93–108 doi: https://doi.org/10.1097/ALN.0000000000004204
2. Weersma RK, Zhernakova A, Fu J Interaction between drugs and the gut microbiome Gut 2020;69:1510-1519.
3. Zhu X., Han Y., Du J., Liu R., Jin K., Yi W. Microbiota-gut-brain axis and the central nervous system. Oncotarget. 2017; 8: 53829-53838. Retrieved from https://www.oncotarget.com/article/17754/text/